According to 2017 census, Pakistan is the 6th
most populous country of the world with population of 207,774,5201. According to WHO, prevalence of diabetes
mellitus in Pakistan is 9.8% and Pakistan has seventh largest diabetic patients
in the world2,3. The prevalence of diabetic retinopathy in Pakistan
is 28.78% among the diabetic population4. Management of diabetic
retinopathy requires long-term patient’s education and comprehensive eye care
to prevent vision impairment.
Imaging has unique and widespread role in
the field of ophthalmology. Imaging is widened to diagnosis, treatment,
documentation, research and learning purposes. Imaging is extensively used for
screening purpose of eye diseases. This is especially true for various retinal
conditions5. It is very expensive and
technically demanding to get good quality ophthalmic images through dedicated
workstations and image capturing units in hospital environment.
Recent development in the hardware and
software of smart phones has spread their use widely. Like all other
professionals, ophthalmologists are not lagging behind in adopting this
revolutionary technology. Smart phones have found their valuable use in the
field of ophthalmology. They are readily available, handy, easy to use and have
great capability for connectivity wirelessly6.
Apart from their conventional role of phone calls and text messaging smart
phones are now able to do multiple tasks like video recording, running soft-wares
and applications, remote connectivity with internet.7,8,9.
Coupled with their portability and
connectivity with other gadgets, smart phone acceptability in the professional
use in the field of ophthalmology is ever increasing10.
Use of smart phone photography is as useful in hospital setting as is in the
remote community setting. For the screening and diagnosis of retinal diseases
particularly diabetic retinopathy by utilizing smart phone, different
modalities are being used. Various attachments have been developed to help
smart phone getting images of the retina. Alternatively, a high power
condensing lens can be used on the principle of indirect ophthalmoscopy to
capture retinal images11,12.
This novel use of smart phone can overcome constrains
of socioeconomic and cultural barriers in providing eye care facilities to
areas where comprehensive eye care facilities are non-existing13. Many
eye diseases causing blindness are preventable like morbidity related to
diabetic retinopathy, glaucoma and age related macular degeneration14.
Effective screening is the key to prevention15. Screening protocols
should address the community as most of the population never visits hospital
before there is permanent damage. Utilization of smart phone fundus photography
to screen and diagnose these crippling diseases has a great potential.
High quality fundus
images can be captured and transferred to distant specialized centres for
expert opinion. This tele-ophthalmic use of smart phone is widely utilized, and
there is much more to come in the future16. The rationale of the
study was to find a cheap, easy to use and reliable tool for screening of
diabetic retinopathy. The purpose of the present study was to compare the reliability
of fundus photography with smart phone in the screening of diabetic retinopathy
with slit lamp microscopy, which is the gold standard.
MATERIAL AND METHODS
This prospective study was conducted in
ophthalmology department of District Head Quarter Teaching Hospital affiliated
with Sahiwal Medical College Sahiwal from January 2017 to December 2017. The
study was approved by the ethical committee of the institution. Consent was
obtained from all patients who were included in the study. Diabetic patients
coming in outpatient department were included in the study. This was cross
sectional study and sampling technique was purposive sampling.
All diabetic patients older than 15 years
of both genders were included. Patients with media opacity were excluded from
the study. Pupillary dilatation was achieved by instilling 1% tropicamide and
10% phenylephrine eye drops that were repeated twice after five minutes
interval. After full dilatation of the pupil fundus photographs were taken with
the help of smart phone and 20 diopter condensing lens. Images of posterior
pole, superior, nasal, inferior and temporal periphery were captured. Smart
phone used for this purpose was Samsung galaxy N9000. Images were taken using a
resolution of 1920×1080. Afterwards patients went through comprehensive eye
examination on slit lamp. Fundus photographs taken by smart phone were sent by
whatsapp to one specialist (ML). Slit lamp examination was performed by another
specialist (AZ). Findings were recorded according to a specially designed
proforma. Both specialists were unaware of each other’s findings. Findings were
categorized on the presence or absence of microaneurysms, exudates, retinal
thickening, haemorrhages, intra-retinal micro-vascular changes,
neovascularization of retina and optic disc. Each specialist individually
placed patients into following categories based on his findings: no diabetic
retinopathy, non-proliferative diabetic retinopathy, proliferative diabetic
retinopathy and clinically significant macular oedema.
Age was presented as
mean and standard deviation while gender was presented as percentage. Ƙ statistics
was used to assess agreement between smart phone and slit lamp findings.
Sensitivity, specificity, positive predictive value, negative predictive value
and diagnostic accuracy were calculated using slit lamp examination as gold
standard. Statistical analysis was performed using statistical programme for
social sciences (SPSS version 21).
RESULTS
There were 250 eyes of
125 diabetic patients in the present study. Mean age was 52.11 ± 11.33 years. There
were 136 (54.4%) males and 114 (45.6%) females.
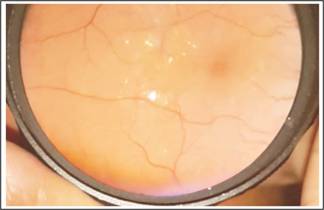
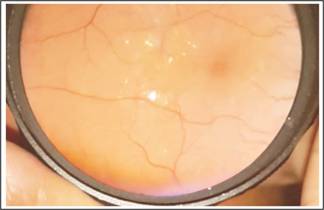
Fig. 1: Retinal thickening, hard exudates and clinically significant
macular oedema
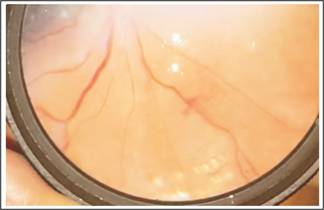
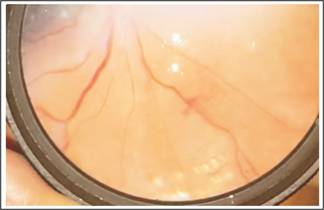
Fig. 2: Neo vascularization elsewhere
and laser marks.
Table 1 shows frequency
of findings along with agreement value between the two groups. Table 2 gives the
sensitivity, specificity, positive predictive value, negative predictive value
and diagnostic accuracy by using smart phone fundus photography for diagnosis
of diabetic retinopathy with slit lamp examination as gold standard.

Fig. 3: Fibrous tractional fold at disc and macula along with neo
vascularization at disc.

Fig. 4: In a silicone oil filled eye there is neo vascularization at disc
and neo vascularization elsewhere.

Fig. 5: Massive plaque exudative
maculopathy.

Fig. 6: Asteroids hyalosis.
DISCUSSION
Diabetic retinopathy is a potentially
blinding condition. Timely diagnosis and appropriate treatment is of paramount
importance to lessen the morbidity of this disease. Traditional fundus imaging
cameras are costly, and they require dedicated environment for their operation17.
There is a need for some alternative that is cheap, readily available, practical
in community settings and has connectivity through telemedicine to specialist
centres if we want to extend our health care services to underserved areas of
the community18.
In the present study, 250 eyes of 125
diabetic patients were screened with the help of smart phone fundus
photography. Slit lamp examination was used as gold standard to diagnose
diabetic retinopathy. Sensitivity, specificity, positive predictive value,
negative predictive value and diagnostic accuracy of smart phone fundus photography
in diagnosis of clinically significant macular oedema was 82.6%, 99.55%, 95%,
98.26% and 98%. Our findings are comparable to the results presented by Russo A
and co-authors. They reported 81% sensitivity and 98% specificity of diagnosing
clinically significant macular oedema with the help of smart phone. In their
study, agreement between examined techniques was 0.79 as compared to 0.87 in
our study. However, Russo and co-authors used D-Eye system as smart phone
camera attachment as compared to 20 diopter condensing lens used in our study.
Our approach utilized the principle of indirect ophthalmoscopy to capture
retinal images. Flashlight of smart phone provided the light source to
illuminate the retina.
Work of Maamari et al17 showed the
quality of retinal images captured with the help of smart phone using 20
diopter condensing lens were of high quality to detect retinal changes.
Smart phone fundus imaging yields high
quality photographs that are comparable to that obtained through fundus camera19.
Like any other skill quality of images captured with smart phone improves with
practice and experience of the examiner. Light exposure by smart phone camera
is very less as compared to indirect ophthalmoscope light, making it a safe
technique in terms of retinal light toxicity20. This decreased light
intensity is more comforting for the patient but at the same time, it makes it
difficult to get fundus images in the presence of media opacity.
Advantages of capturing retinal images with
smart phone are many. Smart phone is an economical device that is readily
available in almost every setting of our community. Moreover, its acceptability
among doctors and public is very high. It needs no extra expensive attachments.
It is true when high power condensing lens is used to take photographs. Nurses,
community health workers and paramedics can be trained to capture images and
send these images through whatsapp or email to retinal specialist located in
specialist centres for expert opinion.
There are limitations of our study. The field
of view by smart phone fundus imaging is less as compared to that obtained by
slit lamp fundus examination that is gold standard. Stereopsis is lacking in
fundus images by smart phone. Moreover, examiner practice is required before
getting high quality images by smart phone. Patient’s cooperation is very
important in getting good images.
Nonetheless smart phone
fundus photography is a promising technique that makes it possible to get high
quality retinal images to detect retinal changes in population of remote and
less served areas. Use of tele-ophthalmology in combination with smart phone
fundus imaging can open a new prospect for screening and diagnosis of
potentially blinding diabetic retinopathy.
Author’s Affiliation
Dr. Ahmad Zeeshan Jamil
MBBS, MCPS, FCPS, FRCS,
FCPS (VRO)
Associate Professor of
Ophthalmology, Sahiwal Medical College, Sahiwal.
Dr. Muhammad Luqman Ali
Bahoo
MBBS, FCPS, FICO, FACS,
Fellowship Refractive
and Cornea Surgery
Assistant Professor &
Head of Ophthalmology, Shahida Islam Medical College, Lodhran.
Dr. Muhammad Younis
Tahir
MBBS, FCPS, Fellowship
in Vitreoretina
Assistant Professor of
Ophthalmology, Quaid e Azam Medical College, Bahawalpur.
Dr. Fazal Shah Shirazi
MBBS, DOMS, MCPS
Consultant Ophthalmologist,
District Head Quarter Teaching Hospital Sahiwal
Role of Authors
Dr. Ahmad Zeeshan Jamil
Concept and design of
study, Interpretation of data
Dr. Muhammad Luqman Ali Bahoo
Drafting and critical
version of intellectual content
Dr. Muhammad Younis
Tahir
Statistical analysis,
manuscript writing, proof reading
Dr. Fazal Shah Shirazi
Literature search and
drafting of article
REFERENCES
1.
Pakistan
bureau of statistics. Province Wise Provisional Results of Census – 2017.
Available at:
http://www.pbs.gov.pk/sites/default/files/PAKISTAN%20TEHSIL%20WISE%20FOR%20WEB%20CENSUS_2017.pdf
[Accessed on 25/05/2018].
2.
Pakistan-World
Health Organization-Diabetes country profiles, 2016. Available at:
http://www.who.int/diabetes/country-profiles/pak_en.pdf?ua=1
[Accessed on 26/05/2018]
3.
Shera AS, Jawad F, Maqsood A. Prevalence of diabetes in Pakistan. Diabetes Res Clinical Prac
2007; 76 (2): 219-22.
4.
Mumtaz SN, Fahim MF, Arslan M, Shaikh SA, Kazi U, Memon MS. Prevalence of diabetic retinopathy in Pakistan: A systematic
review. Pak J Med Sci. 2018; 34 (2): 493-500.
5.
Nazari KH, Nakatsuka A, El-Annan J. Smart phone Fundus Photography. Journal of Visualized
Experiments: 2017; (125) :55958.
6.
Lord RK, Shah VA, San Filippo AN, Krishna R. Novel Uses of Smart phones in Ophthalmology. Ophthalmology, 2010;
117 (6): 1274-.e3.
7.
Zvornicanin E, Zvornicanin J, Hadziefendic B. The Use of Smart phones in Ophthalmology. Acta Informatica
Medica. 2014; 22 (3): 206-9.
8.
Tahiri HR, El Sanharawi M, Dupont-Monod S, Baudouin C. Smart phones in ophthalmology. Journal francais d'ophtalmologie.
2013; 36 (6): 499-525.
9.
Bastawrous A, Cheeseman RC, Kumar A. iPhones for eye surgeons. Eye, 2012; 26 (3): 343-54.
10.
Russo A, Morescalchi F, Costagliola C, Delcassi L, Semeraro F. Comparison of smart phone ophthalmoscopy with slit-lamp
biomicroscopy for grading diabetic retinopathy. Am J Ophthal 2015; 159 (2): 360-4.e1.
11.
Haddock LJ, Kim DY, Mukai S. Simple, inexpensive technique for high-quality smart phone fundus
photography in human and animal eyes. J Ophthalmol. 2013; 2013: 518479.
12.
Myung D, Jais A, He L, Blumenkranz MS, Chang RT. 3D printed smart phone indirect lens adapter for rapid, high
quality retinal imaging. J Mob Technol Med. 2014; 3 (1): 9–15.
13.
Chow SP, Aiello LM, Cavallerano JD, Katalinic P, Hock K, Tolson A,
et al. Comparison of non-mydriatic
digital retinal imaging versus dilated ophthalmic examination for non-diabetic
eye disease in persons with diabetes. Ophthalmology, 2006; 113 (5): 833-40.
14.
Mohamed Q, Gillies MC, Wong TY. Management of diabetic retinopathy: a systematic review. JAMA
2007; 298 (8): 902–916.
15.
Cheung N, Mitchell P, Wong TY. Diabetic retinopathy. Lancet. 2010; 376 (9735): 124–136.
16.
Chhablani J, Kaja S, Shah V. Smart phones in ophthalmology. Indian J Ophthal, 2012; 60 (2): 127-31.
17.
Maamari RN, Keenan JD, Fletcher DA, Margolis TP. A mobile phone-based retinal camera for portable wide field
imaging. Br J Ophthal, 2014; 98 (4): 438-41.
18.
Shanmugam M, Mishra D, Madhukumar R, Ramanjulu R, Reddy S,
Rodrigues G. Fundus imaging with a
mobile phone: A review of techniques. Indian J Ophthal, 2014; 62 (9): 960-2.
19.
Adam MK, Brady CJ, Flowers AM, Juhn AT, Hsu J, Garg SJ, et al. Quality and Diagnostic Utility of Mydriatic Smart phone Photography:
The Smart phone Ophthalmoscopy Reliability Trial. Ophthalmic surgery, lasers
& Imaging retina, 2015; 46 (6): 631-7.
20.
Kim DY, Delori F, Mukai S. Smart phone photography safety. Ophthalmology, 2012; 119 (10): 2200-1;
author reply 1.